The Triple Threat to Women’s Health: HPV, Menstrual Health Challenges, and Period Poverty
In the global pursuit of health equity, women’s health remains at the heart of progress. Among the most pressing yet often overlooked challenges are Human Papillomavirus (HPV), menstrual health, and period poverty. While distinct, these three issues are tightly interwoven, especially for women and girls in underserved communities. Tackling them individually has not yielded the necessary impact. What’s needed is a holistic, integrated approach that bridges education, healthcare, and economic access to uplift women’s health on all fronts.
Understanding HPV and Its Impact
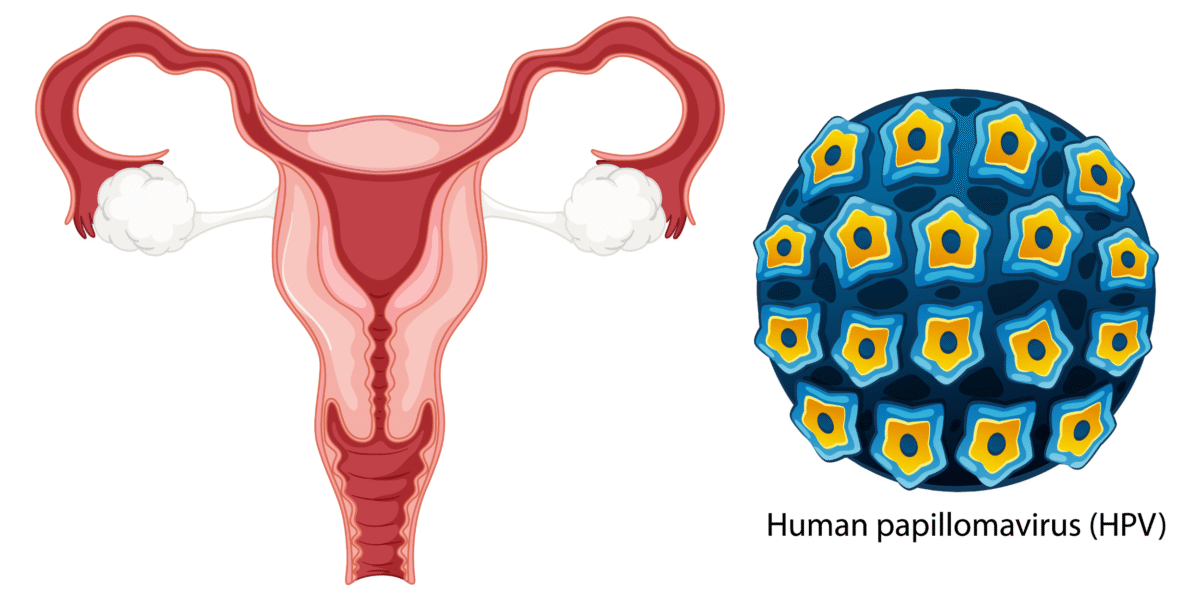
- What is HPV?
HPV, or human papillomavirus, is a common virus, often transmitted through sexual contact, that can lead to various health complications, including cervical cancer, genital warts, and other cancers. Most sexually active individuals will contract HPV at some point, though many will clear the infection naturally.
But can HPV be cleared permanently? In most cases, yes. Especially in individuals with strong immune responses. However, some types of HPV can persist and cause long-term health issues. Is HPV a lifetime infection? Not necessarily, but persistent infections with high-risk strains can last for years and lead to cancer if not detected early.
- What are the symptoms of HPV in a woman?
Often, HPV has no symptoms, which makes regular screening critical. When symptoms do appear, they may include genital warts or abnormal Pap smear results that could indicate precancerous changes in the cervix.
Health Consequences
Persistent human papillomavirus infections can cause cervical cancer, which remains one of the leading causes of cancer-related deaths among women, especially in regions where screening and the human papillomavirus vaccine are limited.
Vaccination Importance
The HPV vaccine is a breakthrough in preventative medicine. It can significantly reduce the risk of HPV-related cancers, especially when administered before the onset of sexual activity. Despite its availability, uptake remains low in many regions due to misinformation, stigma, and lack of access.
One might also ask:
- Can HPV be cured with antibiotics?
No. HPV is a virus, and antibiotics are only effective against bacterial infections. Human papillomavirus infection treatments focus on managing symptoms and preventing complications, such as removing genital warts or treating cervical cell changes, while there’s still no cure for the virus itself.
- How long does HPV last?
The answer is this: For most, it resolves within two years. Others may need long-term monitoring and care.
- How can I boost my immune system to fight HPV?
Maintaining a healthy lifestyle—such as eating nutritious food, getting enough sleep, reducing stress, and avoiding smoking—can help the immune system fight off HPV more effectively.
Menstrual Health: Beyond the Monthly Cycle
Defining Menstrual Health
Menstrual health isn’t just about periods. It encompasses education, access to hygiene products, pain management, and support systems. It is a fundamental part of reproductive and overall health.
Understanding one’s menstrual cycle is key to identifying health changes early, including signs that might indicate an underlying infection like HPV. Irregularities in the menstruation pattern, such as unusually heavy bleeding or spotting between periods, may prompt visits to healthcare providers, leading to earlier detection of cervical issues caused by HPV.
Challenges Faced
Many girls face stigma, bullying, and misinformation around menstruation. In some cultures, having a period is still taboo, leading to isolation and missed school or workdays. Sanitary products remain unaffordable or unavailable to millions.
Health Implications
Without proper menstrual care, individuals risk urinary tract infections, reproductive tract infections, and mental health issues due to embarrassment or social exclusion. Additionally, lack of menstrual health education often translates to a lack of understanding about broader reproductive health issues, including HPV prevention and treatment.
Period Poverty: A Barrier to Health and Education
- What is Period Poverty?
Period poverty refers to the inability to afford or access adequate menstrual products, sanitation facilities, and education. It affects not only physical health but also education, employment, and dignity.
- Consequences
Girls may miss up to 20% of the school year due to lack of menstrual supplies or safe, private restrooms. This affects their performance and long-term career prospects, reinforcing gender inequality.
- Statistics and Case Studies
In the U.S. alone, one in five girls has missed school because they couldn’t afford period products. Globally, over 500 million women and girls lack access to adequate menstrual hygiene facilities.
The Intersection: How These Issues Interrelate
Compounded Challenges
Girls facing period poverty are often the same individuals who lack access to Human Papillomavirus education and vaccination. Without school attendance, they miss critical health information and services, leaving them vulnerable to long-term health risks, including human papillomavirus infection.
Social and Economic Factors
Poverty, gender inequality, and inadequate healthcare systems reinforce this triple threat. Rural areas and low-income urban communities are hit hardest, with limited outreach for both HPV vaccinations and menstrual education.
Case Example
In rural sub-Saharan Africa, integrated school-based programs that provided both HPV vaccines and menstrual kits saw a dramatic drop in absenteeism and an increase in vaccination rates, proving that combined approaches work.
Integrating Solutions: A Holistic Approach
Educational Initiatives
Sexual and reproductive health curricula must include accurate, stigma-free education about menstruation, the menstrual cycle, and HPV. Teachers and parents should be trained to support open conversations and answer important questions such as, What are the symptoms of HPV in a woman?
Healthcare Access
Providing Human Papillomavirus vaccines at schools and clinics while distributing free or subsidized menstrual products can bridge gaps. These must be made accessible, culturally sensitive, and age-appropriate.
Policy Recommendations
Governments should implement policies that:
- Fund free HPV vaccination programs.
- Ensure universal access to menstrual products in schools and public facilities.
- Mandate menstrual health education as part of school curricula.
Community Engagement
Change thrives at the grassroots. Community health workers, faith leaders, and local NGOs can dispel myths, distribute products, and encourage HPV vaccine uptake. Public education should also cover frequently asked questions like Can HPV be cured with antibiotics? and How long does HPV last? to inform and empower communities.
Conclusion
HPV, menstrual health, and period poverty aren’t isolated issues, they form a triad of challenges that demand integrated, compassionate solutions. From expanding human papillomavirus vaccine access to normalizing period conversations and eradicating period poverty, we have the tools and knowledge to make change happen.
Now is the time to act, to advocate for policies that prioritize women’s health holistically and to support initiatives that uplift the lives of women and girls everywhere. The future of women’s health depends on the steps we take today.
Frequently Asked Questions (FAQs)
- Why is it important to integrate HPV vaccination with menstrual health education?
Because both affect adolescent girls, integrating education ensures early awareness, prevention, and empowerment, especially in vulnerable communities. - How does period poverty affect women’s health beyond menstruation?
It leads to physical infections, emotional distress, school dropout, and diminished opportunities, perpetuating cycles of poverty and inequality. - What are effective strategies to combat period poverty in underserved communities?
Providing free menstrual products, investing in sanitation infrastructure, and launching education campaigns tailored to local cultures are key. - How can schools play a role in addressing these health challenges?
Schools can serve as hubs for vaccination, health education, and product distribution, empowering students through awareness and accessibility. - What policies have been successful in integrating these health initiatives?
Countries like Scotland and Kenya have led with free period products and integrated school health programs, showing success through measurable outcomes
All Categories
Recent Posts
Cyclical Breast Pain: What It Is, Why It Happens & How to Feel Better
One Pad, One Girl, One Future: The Impact of Pad a Girl Campaign
PCOS Reality Check: Symptoms, Remedies, Stories
Tags
Give them a helping hand
Every donation fuels our mission to combat period poverty. Your generosity brings us closer to menstrual equity.
+234-909-482-1642
inquiries@blossomflow.org